 What Causes Leaky Gut – Going Beyond Gluten
What Causes Leaky Gut – Going Beyond Gluten
Autoimmunity, including celiac disease, is the modern plague of the industrialized world. Because leaky gut is a major trigger for this massive health crisis, it is important to ask the question…What causes leaky gut?
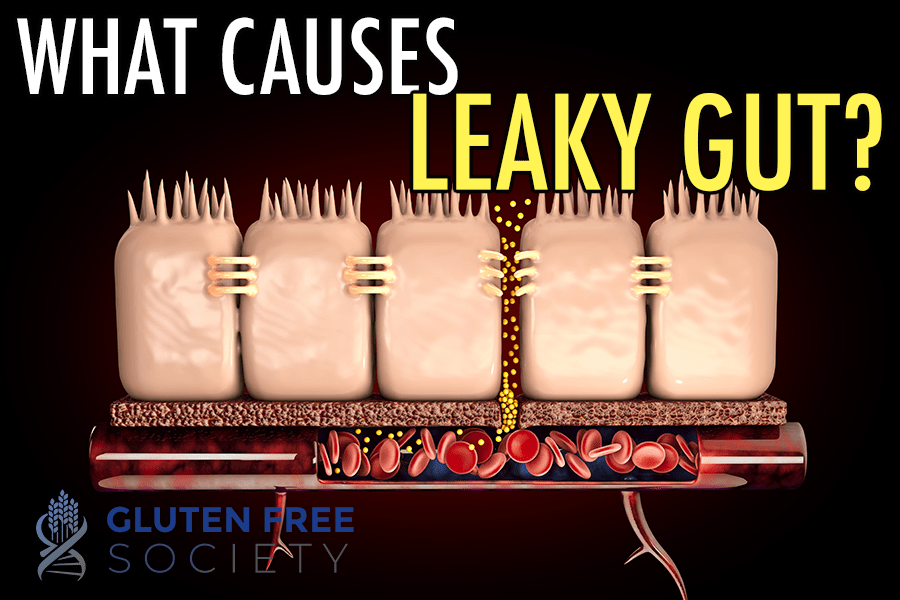
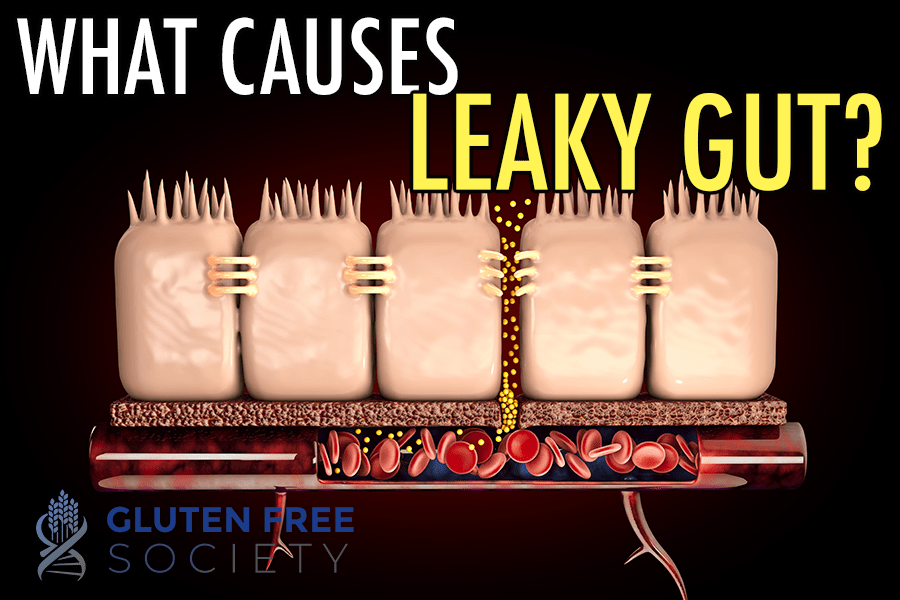
The lining of your small intestine is made up of a single layer of tightly packed cells. The cells are packed tightly together to prevent large particles of food, pathogens, and other potentially harmful substances from entering your bloodstream. Under normal circumstances, water and fully digested nutrients are all that can get through.
However, if the tight junctions between the cells lining your small intestine loosen up, all bets are off. Leaky gut (a.k.a. intestinal hyper-permeability) is what scientists call it. When large undigested food particles, toxins, pathogens, and other substances that you ingest “leak” into your bloodstream. And it’s problematic because your immune system sees these things as foreign invaders. It goes into overdrive and wages a microscopic war against them. The outcome is chronic inflammation.
So if the leak isn’t plugged, it can lead to dysfunction and disease throughout your body. In fact, leaky gut is believed to contribute to the development of autoimmune diseases, including celiac disease.
So the question is…what causes leaky gut? What causes the tight junctions between the cells that line your small intestine to loosen?
Well, there’s more than one answer. And the cause may be different among individuals. However, inflammation, gluten sensitivity, and gut bacteria imbalances are common factors. Keeping these in mind, let’s explore the various known causes of leaky gut in detail…
Food Allergies
Food allergies occur when the immune system reacts to a substance within a food, usually a type of protein, that isn’t inherently harmful under normal conditions. For example, peanuts aren’t poisonous to humans. However, for those with a peanut allergy, eating a peanut may be deadly. Because the immune system overreacts, which ultimately causes swelling and inflammation.
During an allergic food reaction, the immune system activates mast cells in the gut. And mast cells release histamine and other inflammatory compounds that cause allergy symptoms. For example, leukotrienes may be released that can cause your airways to constrict making it difficult to breathe. In your gut, inflammatory compounds released from mast cells (e.g., proteases and cytokines) weaken the integrity of your intestinal lining.
So it’s very clear that eating foods that you’re allergic to can cause a leaky gut. But a leaky gut can also increase the severity of your food allergies as well as cause your body to start reacting to more foods. Because more large food particles are able to enter your bloodstream and interact with your immune system.
Microbial Imbalances & Infections
Gut bacteria play an important role in helping to maintain the integrity of your intestinal lining. There’s evidence suggesting that beneficial bacteria lining your small intestine prevent pathogenic bacteria from colonizing and entering your bloodstream by competing for space and nutrients as well as releasing antimicrobial compounds.
Certain species of bacteria also ferment fiber that you eat to make short-chain fatty acids, which fuel intestinal cells and help maintain the integrity of your intestinal lining.
So if you have an imbalance in your gut where pathogenic bacteria outnumber beneficial bacteria, the lining of your small intestine may weaken and contribute to intestinal permeability.
Viral, bacterial, and parasitic gut imbalances also trigger your immune system, which ultimately causes inflammation. And as I mentioned above, gut inflammation can damage the cells that line your small intestine. This can cause gaps to form directly. But it can also cause other malfunctions that can contribute to leaky gut.
For example, intestinal cells called enterocytes also help prevent the overgrowth of pathogenic bacteria by releasing antimicrobial proteins. So if they stop functioning properly, an overgrowth of pathogenic bacteria is possible.

Prescription & Over The Counter Medications
Many prescription medications and even some over-the-counter drugs can cause intestinal distress and inflammation. Especially when taken long-term. Some commonly prescribed medications that can be problematic include:
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Birth control pills
- Antibiotics
- Immunosuppressants
- Corticosteroids
- Antacids
Unfortunately, these are the same drugs frequently used to treat inflammatory gut conditions. Thus, they can make matters worse if the root cause of inflammation isn’t determined and addressed.
It’s also worth noting that some medications can cause nutrient deficiencies, which can deprive your intestinal cells, alter your gut bacteria, inhibit your immune system, promote inflammation, and lead to dysfunction.
NSAIDs
Prostaglandins are fatty compounds that act like hormones. The effect they have depends on where they’re found. In some cases, prostaglandins can cause pain and inflammation. Thus, NSAIDs primarily work by inhibiting the release of prostaglandins.
However, prostaglandins are also responsible for secreting mucus that protects the lining of your digestive tract. Without this mucosal layer, stomach acid and other acidic substances can cause damage. This is why intestinal bleeding is a known side effect of long-term NSAID use.
NSAIDs are also metabolized in the liver, secreted into bile, and ultimately released into your small intestine. Once there, they’ve been shown to cause oxidative damage to the intestinal cells (a.k.a. enterocytes) that form the tight junctions of your intestinal lining and increase intestinal permeability.
In this observational study, researchers found a strong positive association between frequent aspirin use and the development of Crohn’s disease, an inflammatory bowel disease that can affect both your small and large intestine. In fact, those who took aspirin regularly were 6 times more likely to develop Crohn’s disease than those that didn’t use aspirin.
In addition, regular aspirin use has been associated with a decrease in vitamin C and iron levels.
Vitamin C is a potent antioxidant that protects cells from damage. Iron deficiency as well as excess iron in the gut due to poor absorption can lead to gut bacteria imbalances. And it’s worth noting that vitamin C helps boost the absorption of iron.
Birth Control Pills
Birth control pills aren’t just prescribed to help prevent pregnancy. In many cases, they’re used to help regulate menstruation and reduce PMS symptoms. While this approach may be effective in some cases, it doesn’t solve the underlying hormonal imbalance that’s causing the problem. And it can lead to more problems. Because estrogen has inflammatory effects, which have been shown to increase the risk of inflammatory bowel disease, especially Crohn’s disease.
Oral contraceptives have also been shown to decrease levels of the following nutrients:
- Vitamin B6
- Vitamin B12
- Folate
- Calcium
- Magnesium
- Vitamin C
- Vitamin E
Magnesium is a key player when it comes to immune regulation and inflammation. Plus, deficiencies have been shown to alter the composition of gut bacteria.
Like vitamin C, vitamin E is also a powerful antioxidant.
Antibiotics
Antibiotics are used to treat or prevent infections. However, we know that they alter the composition of your gut bacteria. And these changes can increase the presence of opportunistic bacteria that can cause harm.
Immunosuppressants
Mycophenolic acid (MPA) is a drug used to suppress one’s immune system after organ transplantation. The goal is to prevent the immune system from rejecting a new kidney or liver. But MPA is also used to treat autoimmune diseases, including Crohn’s disease.
Evidence suggests that MPA promotes inflammation in the gut and can cause diarrhea in transplant patients. In an attempt to determine why MPA caused diarrhea, researchers biopsied the colons of patients taking MPA. They found that 79% of the patients studied had colon tissue abnormalities consistent with those with Crohn’s disease, which included active inflammation.
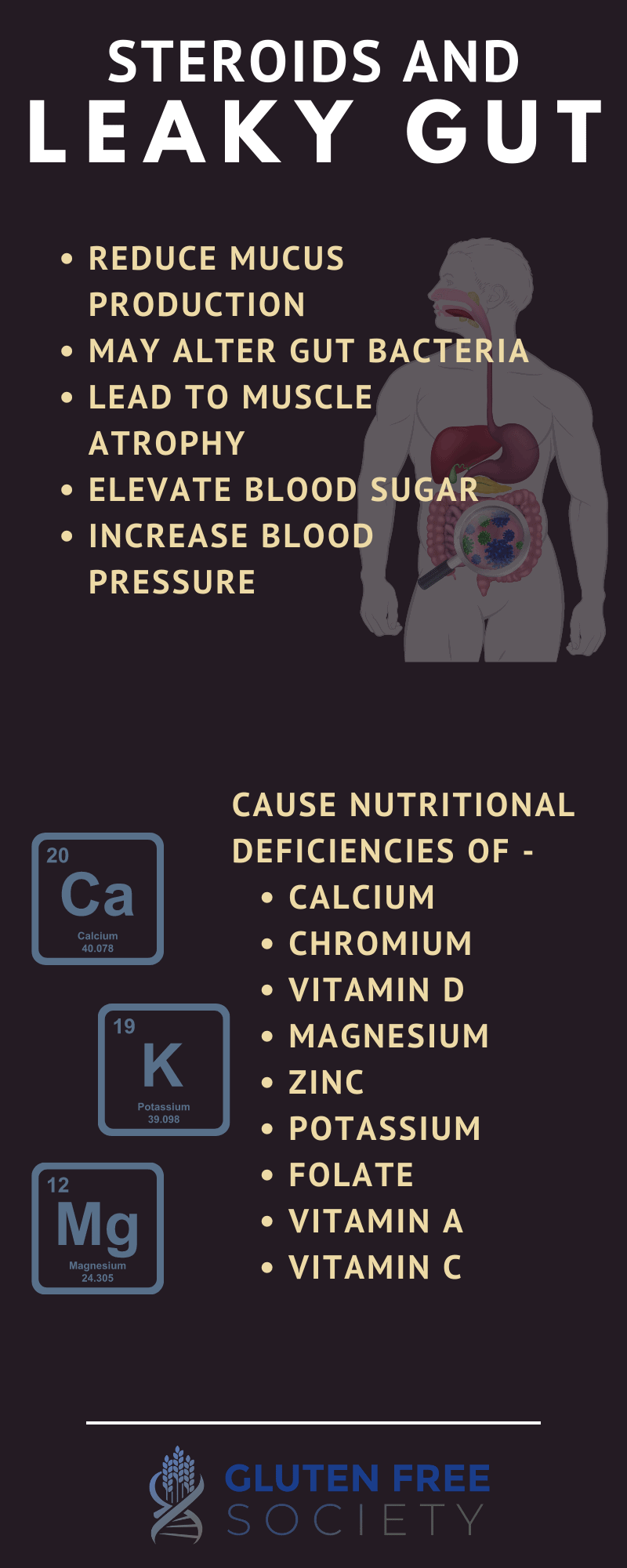
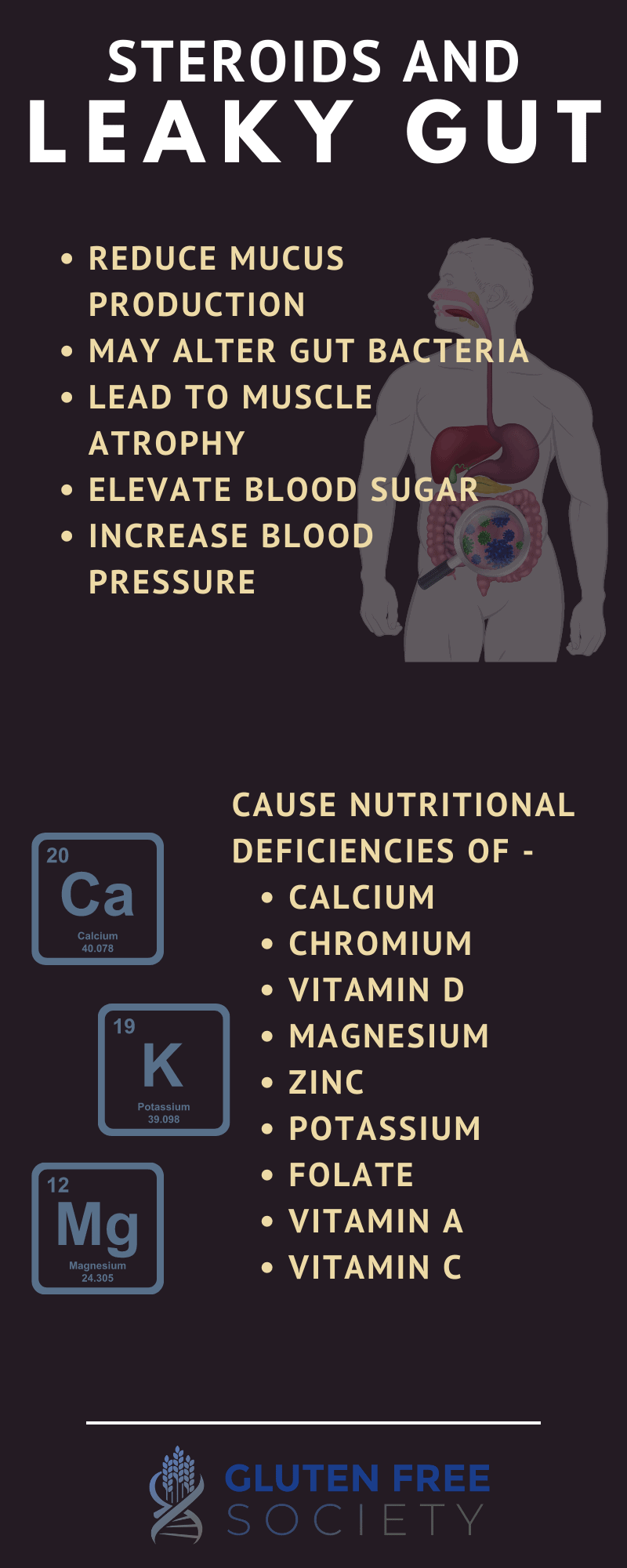
Corticosteroids
Similar to NSAIDs, glucocorticosteroids are often used to reduce inflammation. However, they also reduce the secretion of protective mucus in the gastrointestinal tract. In addition, evidence suggests that they interfere with beneficial bacteria in the gut, which can also reduce the production of mucus as well as promote inflammation.
Corticosteroids can also increase your risk of deficiencies for the following nutrients:
Each of these nutrients are important for gut function, digestive function, immune function, and overall necessary for the body to be able to heal from leaky gut.
Antacids
Antacids are prescribed for chronic acid reflux (a.k.a. GERD). However, shutting down your body’s natural production of stomach acid for an extended period of time has serious consequences.
Stomach acid kills many pathogens before they have a chance to enter your bloodstream. So without it, infections may be more likely. And I’ve already discussed how infections can contribute to leaky gut.
Stomach acid is also necessary to release minerals from the foods you eat as well as successfully digest protein. So without it, mineral and protein deficiencies are possible, which can create many problems.
For example, glutamine is an amino acid (smallest unit of protein) that serves as a fuel source for the cells that line your digestive tract. It’s involved in the maintenance and repair of your gut lining to help maintain its integrity. Glutamine also protects your intestinal cells from damage and helps reduce gut inflammation. In this study, glutamine supplementation was shown to reduce intestinal permeability in burn victims that were under severe stress.
It’s also important to recognize that antacids can lead to numerous nutrient deficiencies, including:
- Vitamin B12
- Vitamin C
- Iron
- Calcium
- Magnesium
- Zinc
Zinc is essential to optimal gut health. It acts as an antioxidant. Plus, deficiencies have been associated with diarrhea and intestinal permeability in children with gastrointestinal diseases in developing countries.
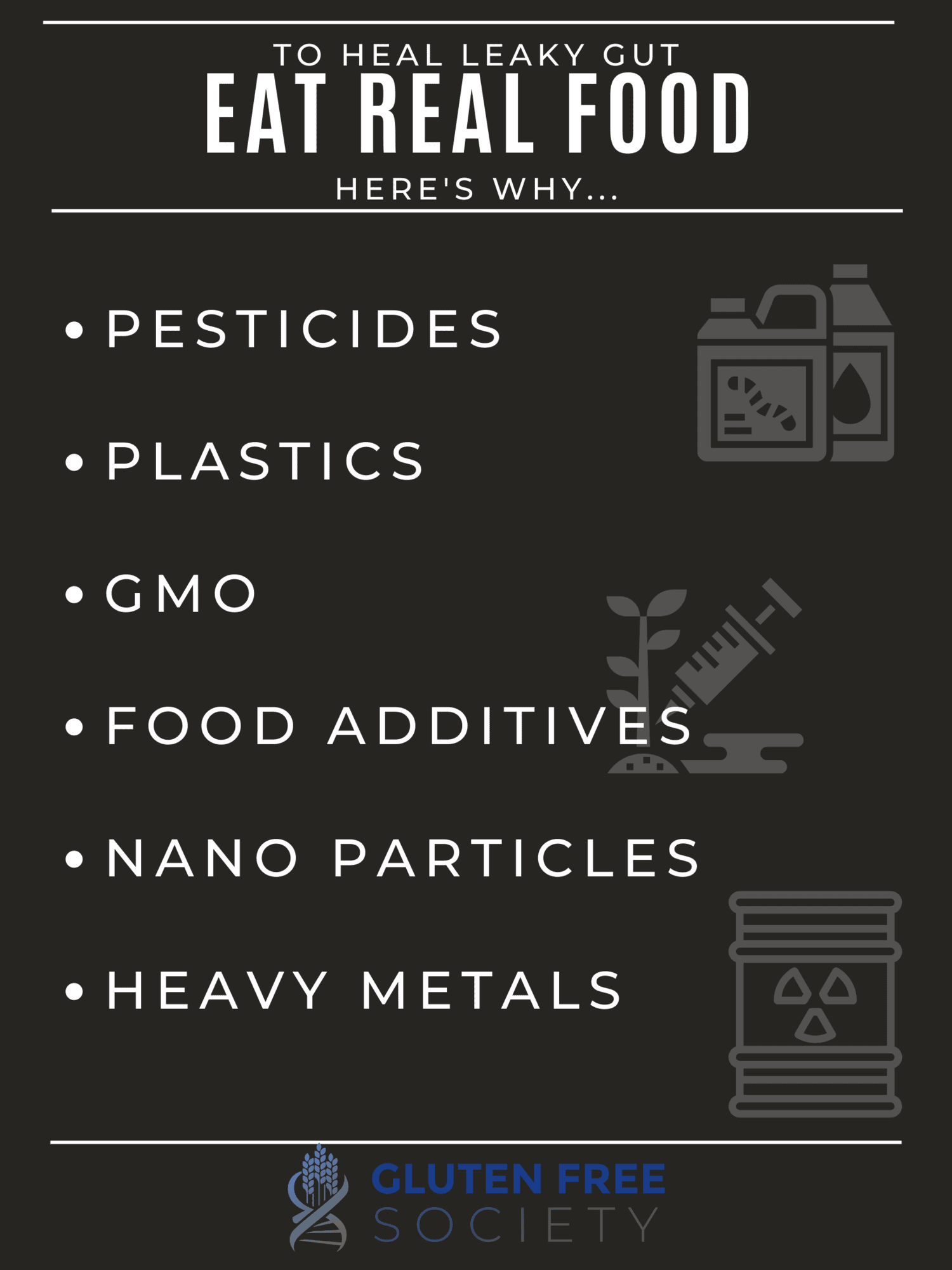
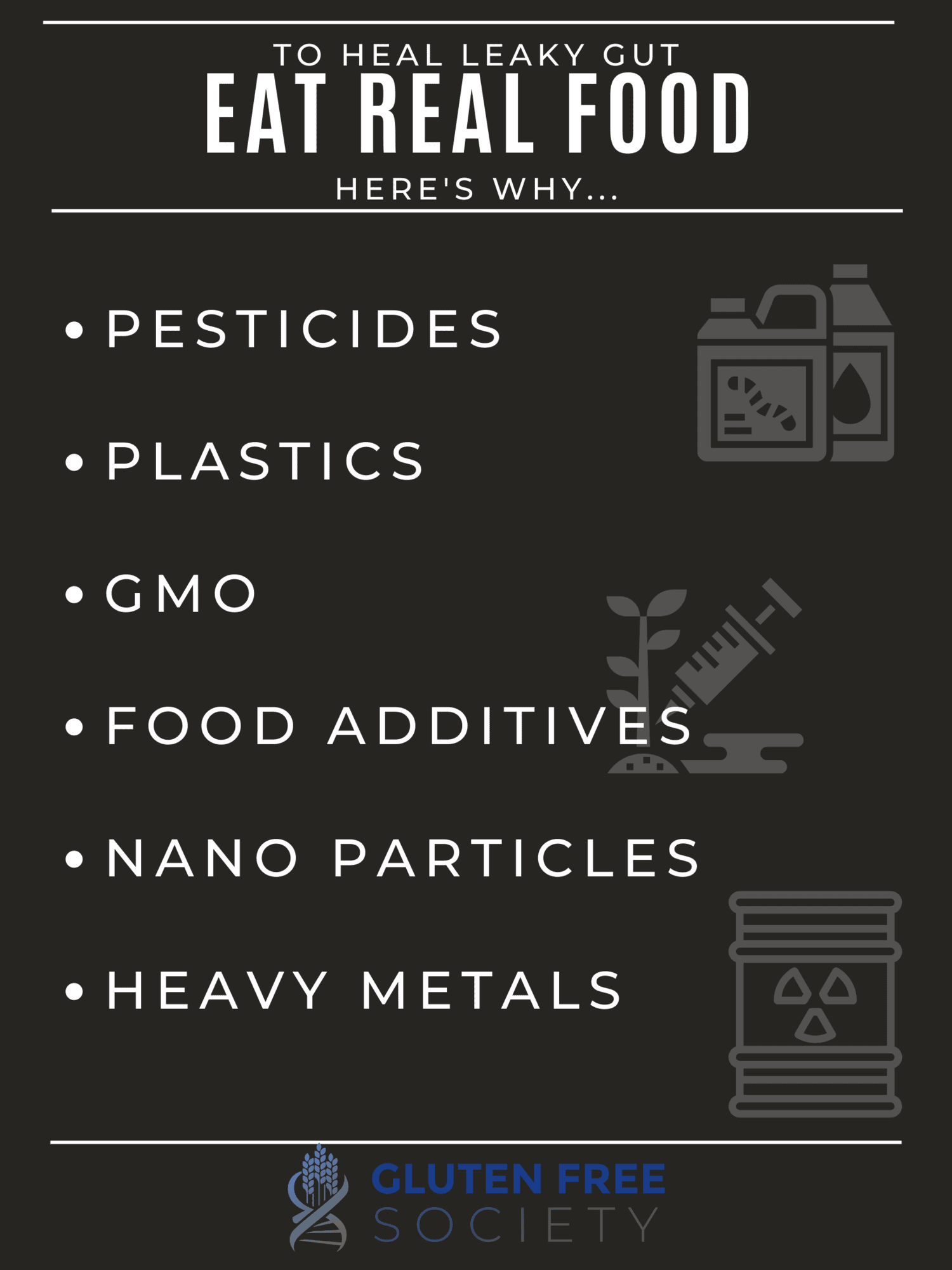
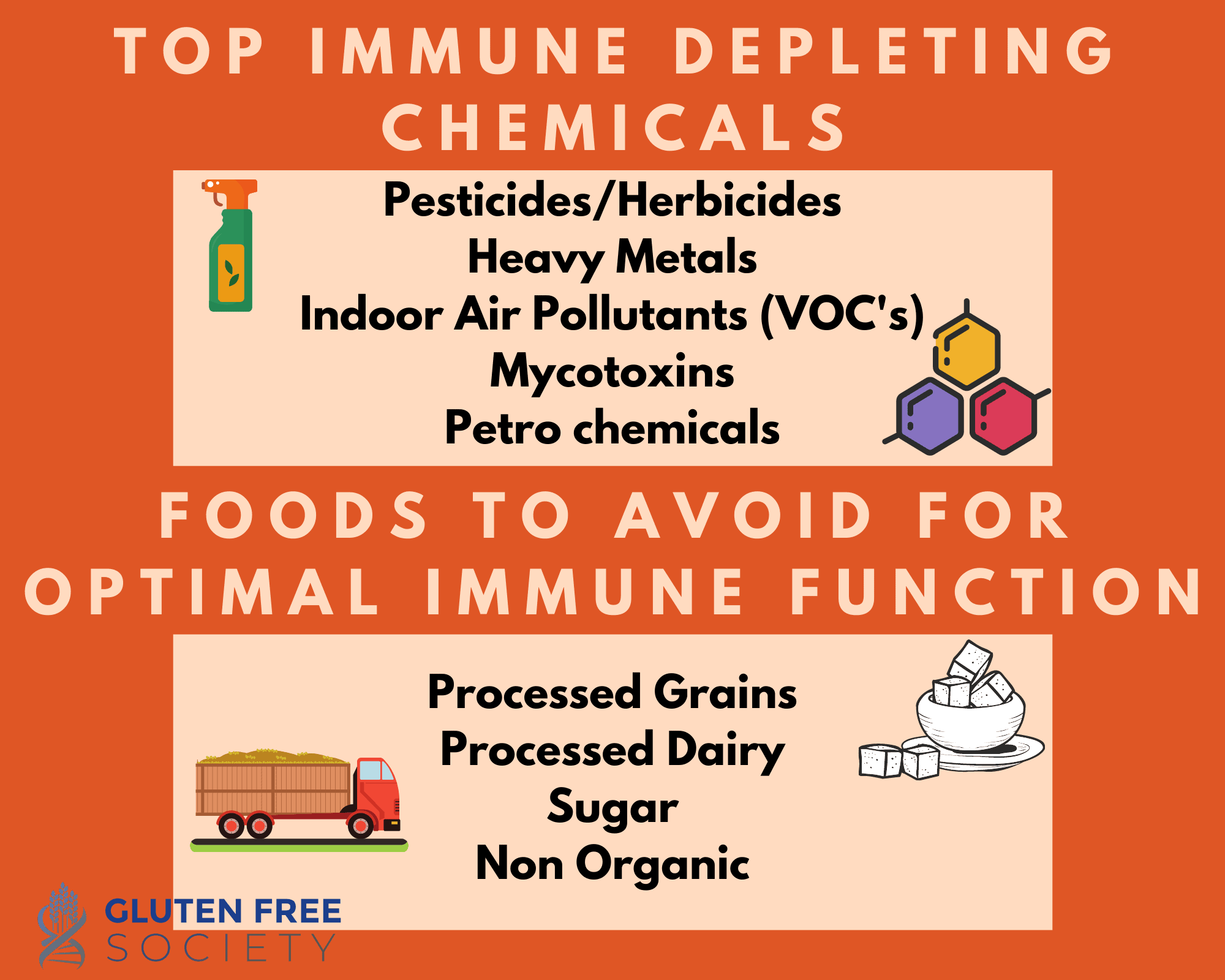
Environmental Toxins
Our environment is filled with toxins at every turn. And many of them make their way into our digestive tract, such as:
- Pesticides
- Plastic chemicals
- Food additives
- Genetically modified foods
- Heavy metals (i.e., lead, mercury, arsenic)
In many cases, the stomach and the intestines are the first major organs that these toxins come in contact with. This is problematic because these toxins can act as free radicals and damage the intestinal cells they come in contact with. Some may also negatively affect your gut bacteria.
Pesticides
Pesticide use is wide-spread around the world. There’s residue on our food as well as in the air we breathe and the water we drink. We’ve been told that low dose exposures aren’t harmful, but that’s not what scientific evidence tells us.
In this study, researchers examined the effects of daily low dose (1 mg/day) exposure to the pesticide chlorpyrifos on cultured human gut bacteria. After 30 days of daily exposure, there was a slight increase in the total count of bacteria.
However, the composition of the bacteria changed for the worse. The population of beneficial bifidobacteria decreased. And the population of potentially harmful gram-negative bacteria increased.
Some species of bacteria moved from one location of the intestines to another. For example, a group known as the Bacteroides moved from the top portion of the colon to the end of the colon.
The diversity of bacteria also decreased. Plus, there was a decrease in the production of short-chain fatty acids.
Other studies (here and here) also reported that low dose exposure to chlorpyrifos altered the gut bacteria in animals, which then caused inflammation and increased gut permeability.
Because of these known effects and others, the use of chlorpyrifos has been limited in the United States. However, it’s still widely used in other parts of the world. And pesticides that have taken its place have shown similar effects. One in particular is glyphosate.
Glyphosate is the active ingredient in the commonly used herbicide Round-Up. It’s not only sprayed on crops to eliminate pests, but it’s also sprayed on wheat to speed up the drying process and increase yield.
There’s mounting evidence showing that glyphosate kills beneficial bacterial species and promotes the growth of pathogenic bacteria. But it’s also been shown to hinder digestion, which can be especially problematic when it comes to gluten.
Gluten is a protein that’s difficult to digest, whether you have a gluten sensitivity or not. But when combined with glyphosate, digesting it becomes even more difficult. Thus, large gluten proteins remain in the gut longer than normal, which can cause the immune system to react and your gut to become leaky. Thus, it’s been suggested that glyphosate could be a factor contributing to the rise in gluten sensitivity and celiac disease.
Plastic Chemicals
Most plastics are made from petroleum. And other chemicals are added to change the properties of the plastic. For example, BPA (bisphenol-A) is used to help harden plastics. But it’s also been found to negatively impact human health. Because it leaches into food and water when they’re stored in plastic.
For our purposes, BPA has the potential to create an overactive immune system via several mechanisms. And when this happens, your immune system may start reacting to food and other inherently non-harmful substances. Your immune system may also start reacting to proteins on your own cells (a.k.a. autoimmunity). These scenarios cause cellular damage and inflammation, which can lead to leaky gut.
Food Additives
Processed foods are packed with ingredients made in a lab. These ingredients have little to no resemblance to real food. And their purpose is to make products look good, smell good, taste good, feel good in your mouth, and last forever on the shelf. Because that’s how they keep you coming back for more.
However, because these ingredients aren’t real food, your body has a hard time processing them. They are foreign chemicals your body must detox. When consumed infrequently in small doses, a healthy detoxification system is able to keep up. However, these days we’re constantly bombarded with chemicals that our bodies must contend with.
Emulsifiers are a category of food additives used to help stabilize products made with a combination of fats and water-based ingredients. They help keep the two from separating as well as improve the texture.
There’s a wide range of emulsifying chemicals in use. Within the food industry, they’re commonly referred to as “surfactants.” And studies have shown they’re directly capable of weakening the layer of mucus that protects the lining of your intestines as well as loosening the tight junctions between your intestinal cells.
There’s also evidence that surfactant-based food additives can cause gut bacteria imbalances. For example, when surfactant-based emulsifiers were given to mice in this study, populations of mucus degrading bacteria grew and led to the development of inflammatory bowel disease.
In this ex vivo (human tissue studied in an external environment) study, emulsifiers caused the growth of pro-inflammatory gut bacteria, which led to intestinal inflammation.
Maltodextrin is another commonly used food additive. It’s made from corn, rice, potato, or wheat starch. And it’s generally used as a thickener. But like emulsifiers, it doesn’t have a good rap sheet when it comes to your gut.
In piglets, it’s been shown to induce necrotizing enterocolitis, which causes bacterial infections and extreme intestinal inflammation.
In this study, mice given maltodextrin experienced changes to their gut bacteria that inhibited them from being able to fight off Salmonella infections.
Another mouse study concluded that maltodextrin decreased the production of protective intestinal mucus, triggered intestinal inflammation, and increased the risk of colitis.
Artificial sweeteners may seem like a miracle, but they can cause harm in numerous ways. When it comes to your gut, studies have shown they can alter the composition of your gut bacteria for the worse as well as promote intestinal inflammation.
For example, this mouse study found that Splenda increased the population of potentially pathogenic gram-negative bacteria, which includes E. Coli, Salmonella, and Helicobacter.
Titanium dioxide is a commonly used white food coloring that may also negatively affect your gut. In this study, researchers looked at the effects of titanium dioxide on mice and human cultured cells from individuals with colitis. They reported that titanium dioxide caused the release of inflammatory compounds in the intestines, which aggravated their condition and increased intestinal permeability.
Meat glue (a.k.a. microbial transglutaminase) is secretly used by food manufacturers to “glue” smaller scraps of meat into one larger chunk. It’s also added to dairy products, such as yogurt and ice cream, to improve their texture. So it helps increase profit. But it may also be destroying the lining of your intestines.
Meat glue alters the physical structure of protein. So when you eat proteins treated with meat glue, they become more difficult to digest. Your body is also less likely to recognize them. So your immune system is more likely to react, which can lead to inflammation and leaky gut.
In fact, evidence suggests the combination of meat glue and gluten proteins may be another factor contributing to the rise of celiac disease, which is closely associated with leaky gut. Essentially, it may increase the likelihood of your immune system reacting to gluten proteins.
Nanoparticles aren’t added to food. They’re used in food packaging as an antimicrobial agent. But like plastic chemicals, they can leach into our food and water.
Animal studies have shown that nanoparticles can cause damage to intestinal cells, intestinal inflammation, and gut bacteria imbalances.
This isn’t an exhaustive list of all the food additives linked to leaky gut. But I hope it’s clear that these lab-made ingredients may have benefits when it comes to taste, texture, and shelf-life. But we can’t ignore the potential dangers. Food additives are one of the many reasons I don’t recommend eating processed foods.
Genetically Modified Foods (GMOs)
Genetically modified foods are crops that have been altered genetically to have specific traits. For example, bacterial genes may be added to certain crops that cause the crops to produce proteins that kill insects.
This may sound like a good thing. But studying the health effects of genetically modified foods in humans is difficult to do. Therefore, we don’t fully understand the potential for harm. However, research suggests there may be unintended consequences.
For example, modifying a crop’s DNA may cause the plant to produce “unnatural” compounds. It’s possible that your immune system views these new compounds as toxins or allergens.
In fact, our food supply is flooded with genetically modified corn and soy. They’re widely used in processed food. Plus, many food additives are made from genetically modified corn, including maltodextrin and high fructose corn syrup. Thus, our exposure is high. And it’s interesting that corn and soy are also two of the most allergenic foods.
Plants may also produce more or less of a specific natural compound. And consuming them in abnormally high or low concentrations may create a problem.
In addition, maybe you’ve heard of “Round-up Ready” crops? Essentially, they’re crops genetically modified to withstand heavy applications of the herbicide glyphosate. And I’ve already discussed how glyphosate can cause leaky gut.
Heavy Metals
Like many of the toxins discussed above, heavy metals have been shown to disrupt the balance of gut bacteria in animal studies.
Again, we’re not talking about high doses of heavy metals. In this study, mice were given a low dose of cadmium. Similar to “acceptable” levels found in drinking water. They found their gut bacteria were negatively impacted, which caused intestinal permeability. As a result, higher levels of cadmium were found in the livers of the mice, which then caused liver damage.
Aggressive Exercise
I think all experts would agree that exercise is a good thing. But just like everything else, overdoing may be harmful. In fact, this systematic review found that as the duration and intensity of exercise increased, so did the potential for intestinal injury and leaky gut. Especially among those with existing gut conditions.
The condition is referred to as “exercise‐induced gastrointestinal syndrome.” And there are two proposed pathways.
The first pathway involves stress. Physical activity activates your body’s stress response. For short stints, this is a good thing. But exercising at high intensities for an extended period of time keeps your body in the fight or flight mode longer than desired. Stress hormones cause your food to move more slowly through your digestive tract, which can cause digestive distress (e.g., bloating and gas). Exercise-induced stress can also prevent food from being fully digested and absorbed. So food particles may sit for too long and ultimately cause cellular damage and lead to intestinal permeability.
The second pathway involves blood flow. More specifically, aggressive exercise can reduce the amount of oxygen delivered to intestinal cells, which can cause cellular damage and dysfunction.
Stress
Excessive exercise is one form of stress. But there are many other types of stress we’re faced with. Unfortunately, many people today experience chronic stress. Whether it be physical stress (e.g., disease, trauma, or injury), psychological stress, or both.
Studies have shown trauma from surgery or serious injuries can induce intestinal permeability. And it’s well known that the stress endured by lab animals during transport impairs the function of their intestinal barrier.
In this study, rats had 1 hour daily sessions where they were surrounded on all sides by water for 5 days. This situation causes a mild degree of stress. Researchers believe it best mimics the level of everyday stress in humans (as opposed to acute stress).
The rats lost weight. Their food intake went down. And intestinal permeability increased. The researchers suggest mast cells had something to do with it. Essentially, stress can activate mast cells in your gut. And remember that mast cells release inflammatory compounds that can weaken the integrity of your intestinal lining.
Studies have also found that stress can alter your gut bacteria. This study found stress in rats caused bacteria to stick to the mucus layer of their intestines, which can lead to an infection. And this study showed that when infant monkeys were separated from their mothers, their population of beneficial Lactobacillus gut bacteria decreased and their susceptibility to gut infections increased.
Potatoes (What?!?)
I already know what you are thinking…”No way I am giving up potatoes!”
Animal studies have found that compounds (a.k.a. glycoalkaloids) in potatoes can make intestinal cell membranes permeable to undesired substances, which can lead to leaky gut.
Interestingly, these glycoalkaloids are concentrated when potatoes are fried. Researchers suggest this may be why the prevalence of inflammatory bowel disease is highest in countries that consume the largest quantities of fried potatoes.
As a nightshade, potatoes are commonly removed from the diet of those with autoimmune diseases lending toward great success and improvements – especially in autoimmune arthritis.
Gluten – The Mother of Leaky Gut
This conversation wouldn’t be complete without discussing gluten. For gluten-sensitive individuals, gluten causes leaky gut in the following ways.
- When intestinal cells interact with gluten proteins, the cells produce and secrete a protein called zonulin. And zonulin is directly responsible for regulating the tight junctions between your intestinal cells. So as zonulin production increases, the tight junctions between your intestinal cells loosen and cause leaky gut. In this study, researchers found that a gluten-free diet significantly reduced zonulin levels as well as anti-gluten antibodies in those with non-celiac gluten sensitivity. Zonulin levels also coordinated with levels of autoimmune antibodies used to diagnose celiac disease. And the researchers found evidence of genetic factors that influence how well zonulin levels respond to a gluten-free diet.
- When you eat gluten, your immune system is triggered. Mast cells in your gut are activated. And these things lead to inflammation and cellular damage.The immune reaction and resulting damage that occurs in response to gluten is a form of physical stress.
- Since gluten causes intestinal damage and inflammation, it negatively impacts your ability to digest food and absorb nutrients. But the damage isn’t limited to your intestines. Organs responsible for producing your digestive juices may also be affected, which can further hinder digestion. So food sits for too long in your digestive tract causing distress and triggering your immune system. Nutrient deficiencies also occur, which cause physical stress. Plus, a wide range of nutrients is needed to maintain a healthy gut.
- The destruction caused by gluten can lead to gut bacteria imbalances, which can trigger inflammation and microbial imbalance. Plus, medications used to treat symptoms associated with gluten sensitivity can alter the composition of your gut bacteria as previously discussed.
- Gluten-rich foods are often highly processed, nutrient-deficient, and packed with pesticides, plastic chemicals, and food additives. They’re also high in starch and sugar, which can contribute to gut bacterial imbalances and yeast overgrowth.
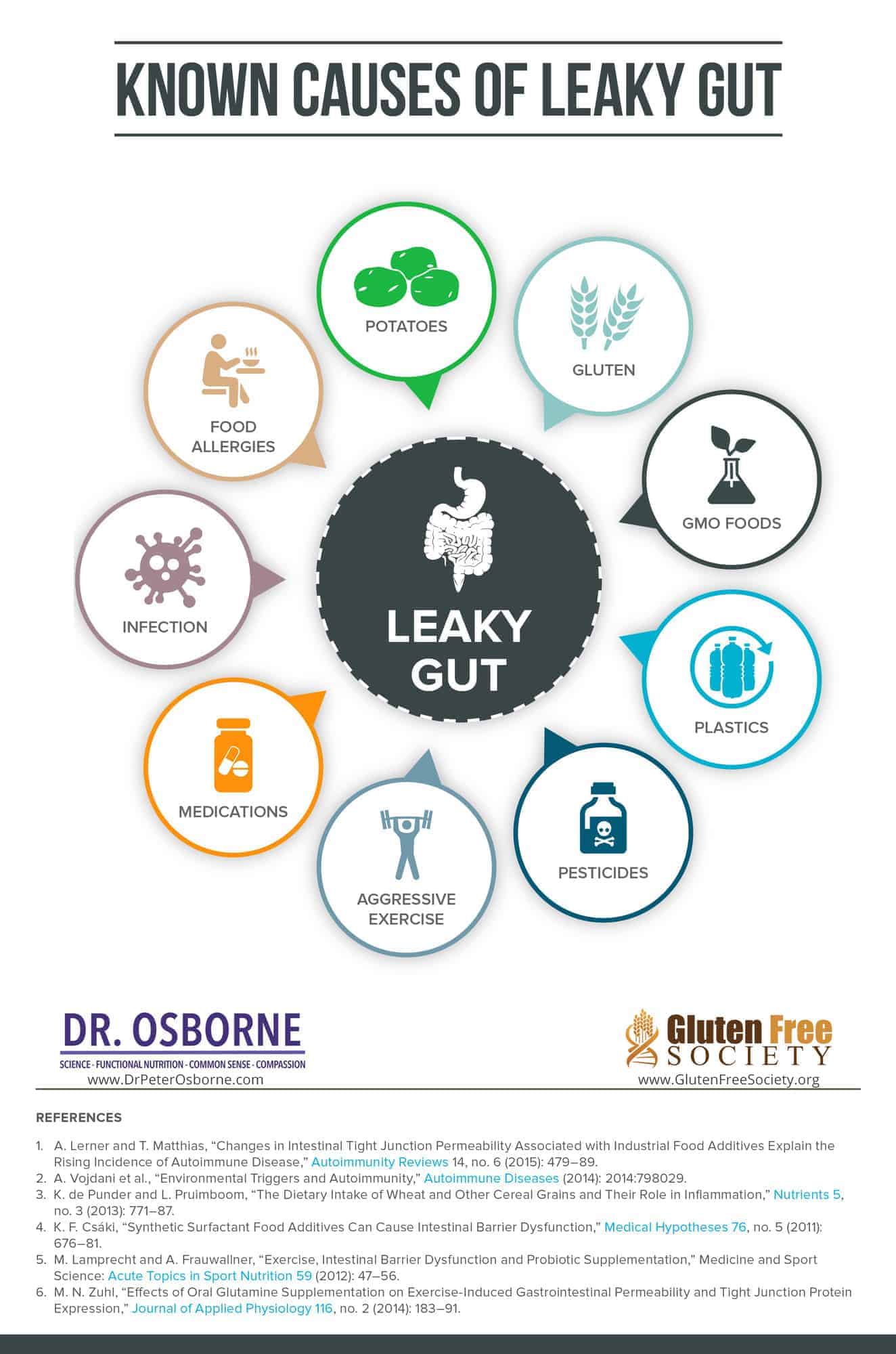
The diagram below simply summarizes the most common causes of leaky gut. Make sure you share it with loved ones – especially if they are suffering with autoimmune disease.
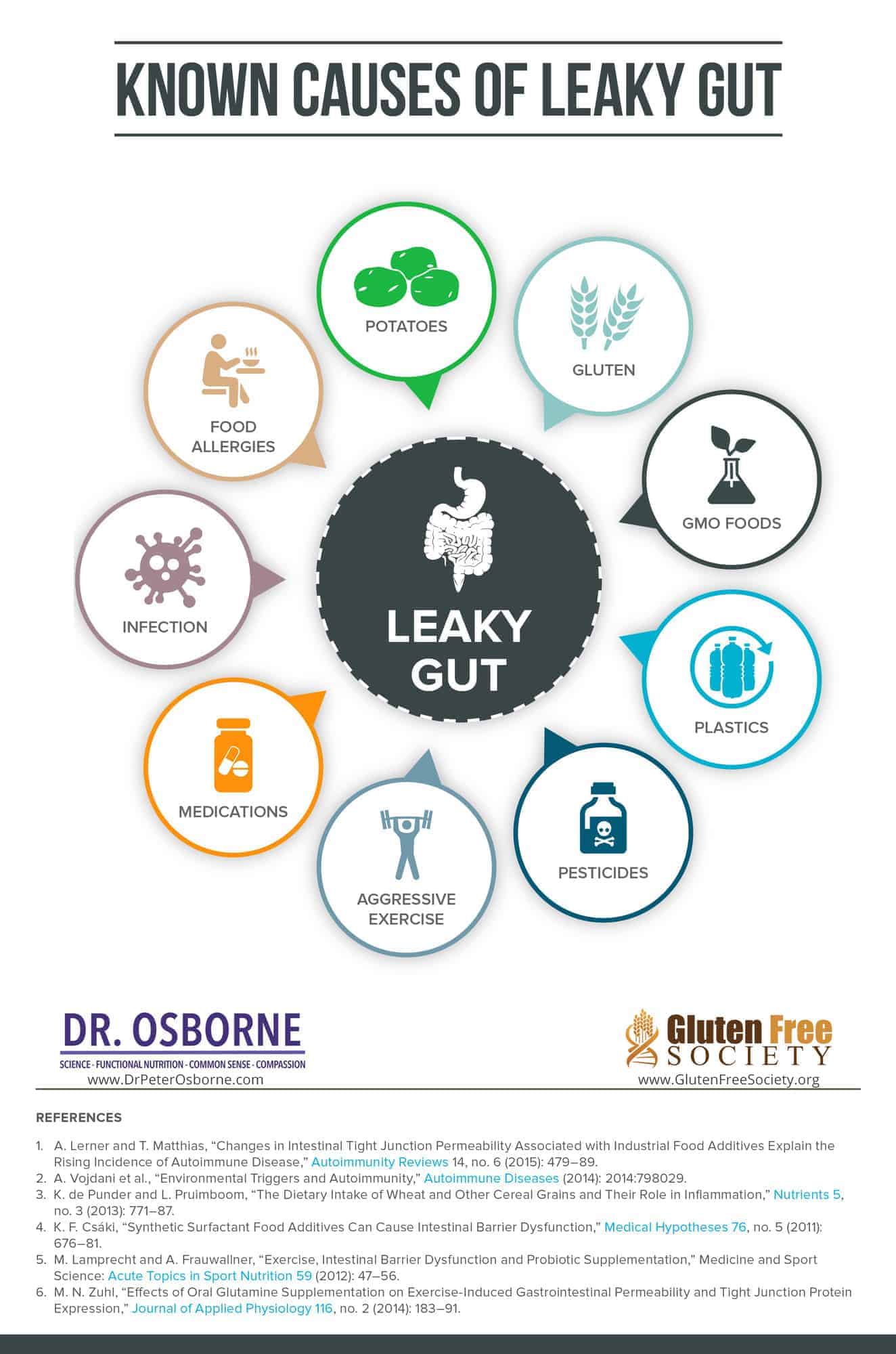
What Causes Leaky Gut?
Leaky gut is on the rise. And we know, in most cases, it’s caused by the food you eat, the lifestyle you lead, and the chemicals in our environment. Because it is a trigger for the development of autoimmune disease, and because autoimmunity is the leading cause of death in females under 65, it is vital to understand what you can do to take control of your health.
The good news is you have the power to prevent it or tighten the gaps if you suspect your gut is leaking. Eating a diet rich in whole foods, reducing stress, and ditching chemicals, gluten, and grains is a great place to start.
DId you overcome leaky gut? Leave your comments below…
The post What Causes Leaky Gut – Going Beyond Gluten appeared first on Gluten-Free Society.
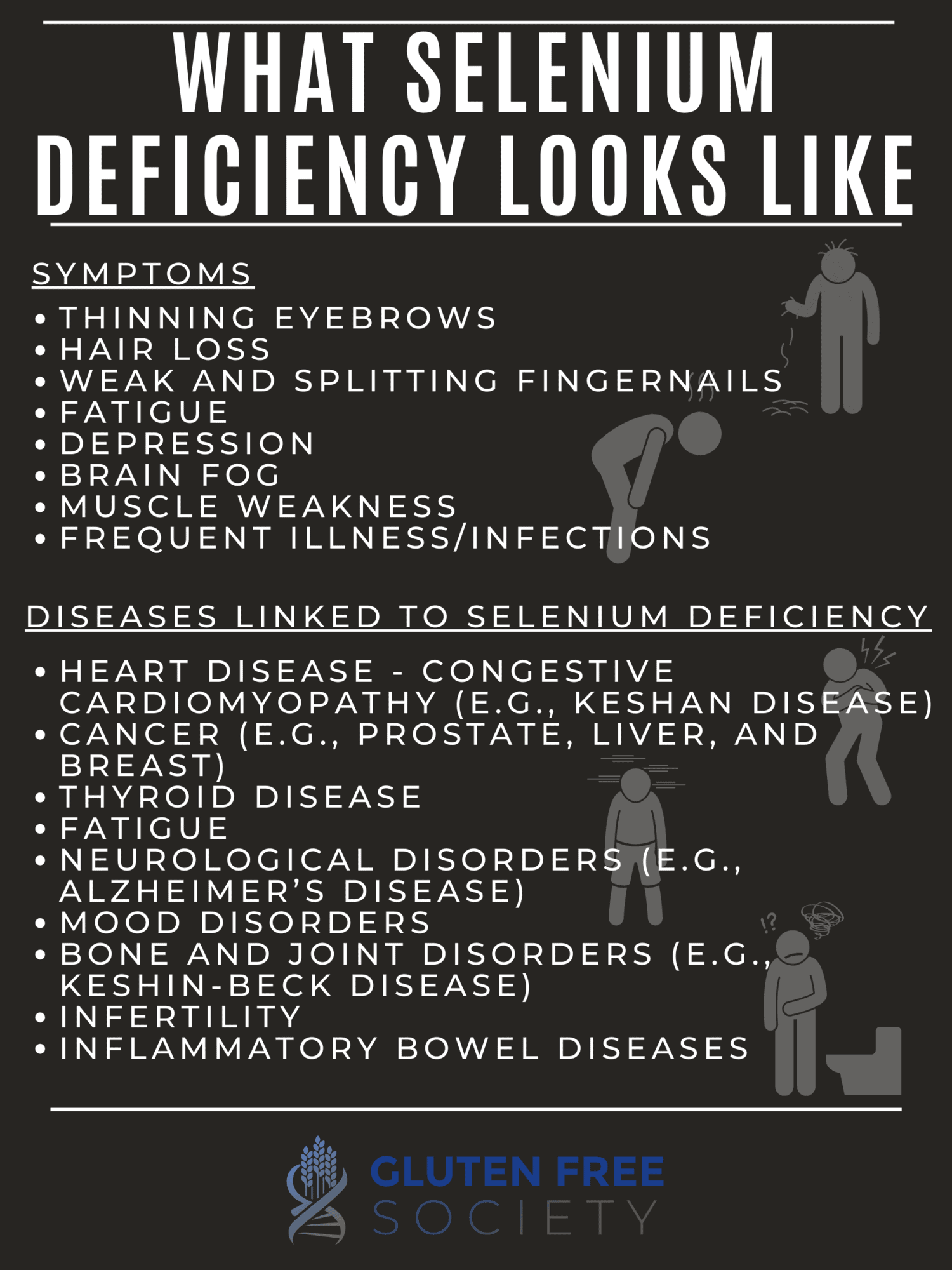
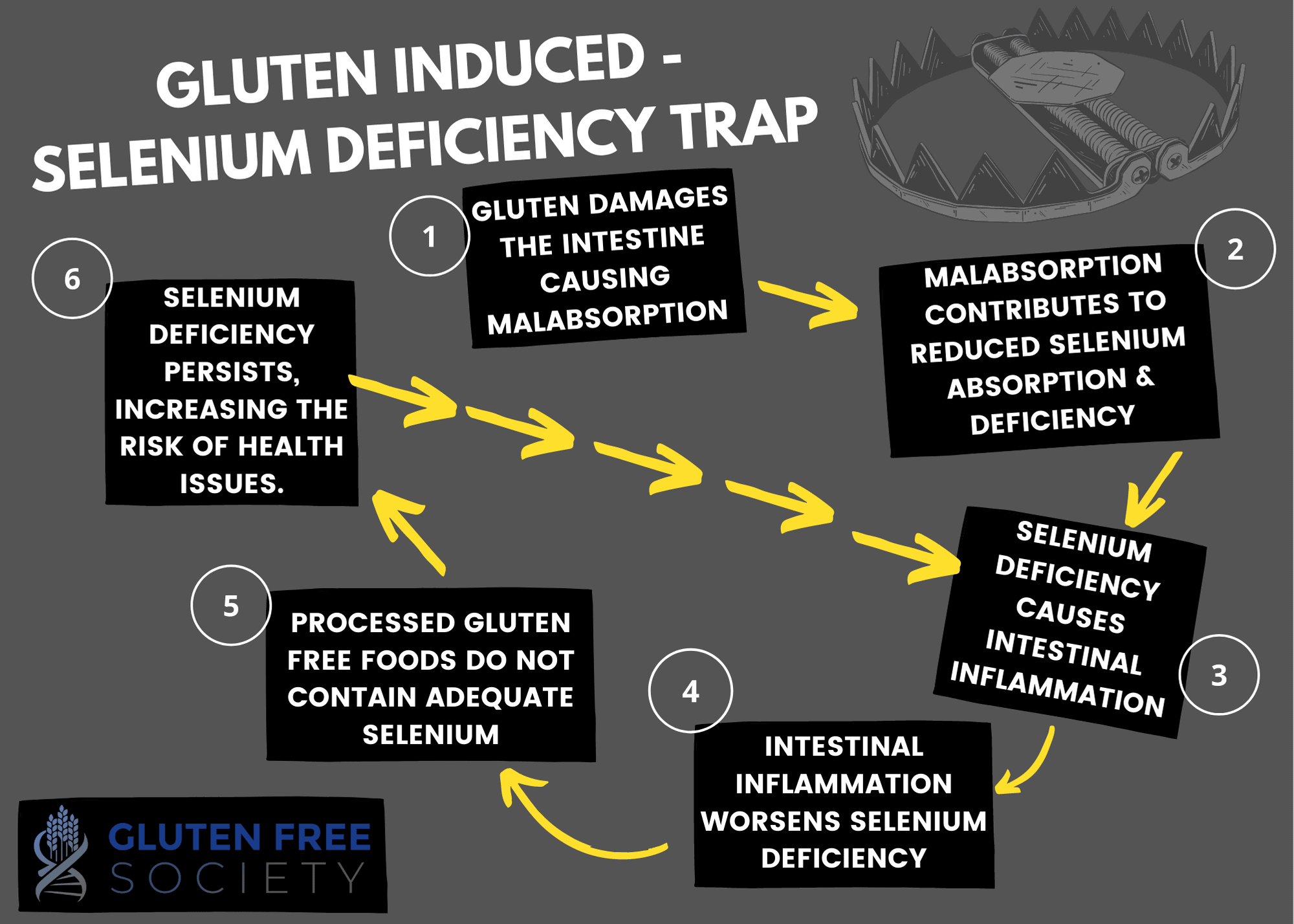
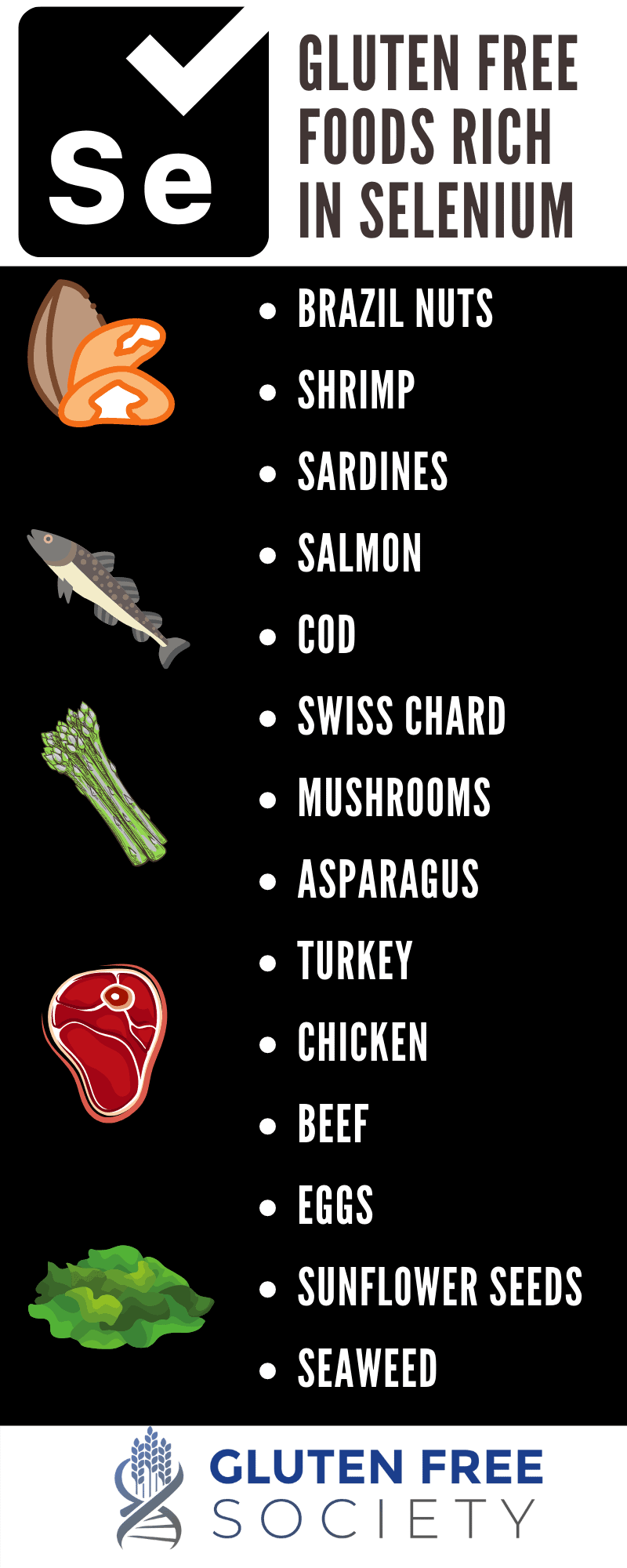
 Gluten Sensitivity, Celiac Disease, and Selenium Deficiency
Gluten Sensitivity, Celiac Disease, and Selenium Deficiency 
 Gluten & Copper Deficiency
Gluten & Copper Deficiency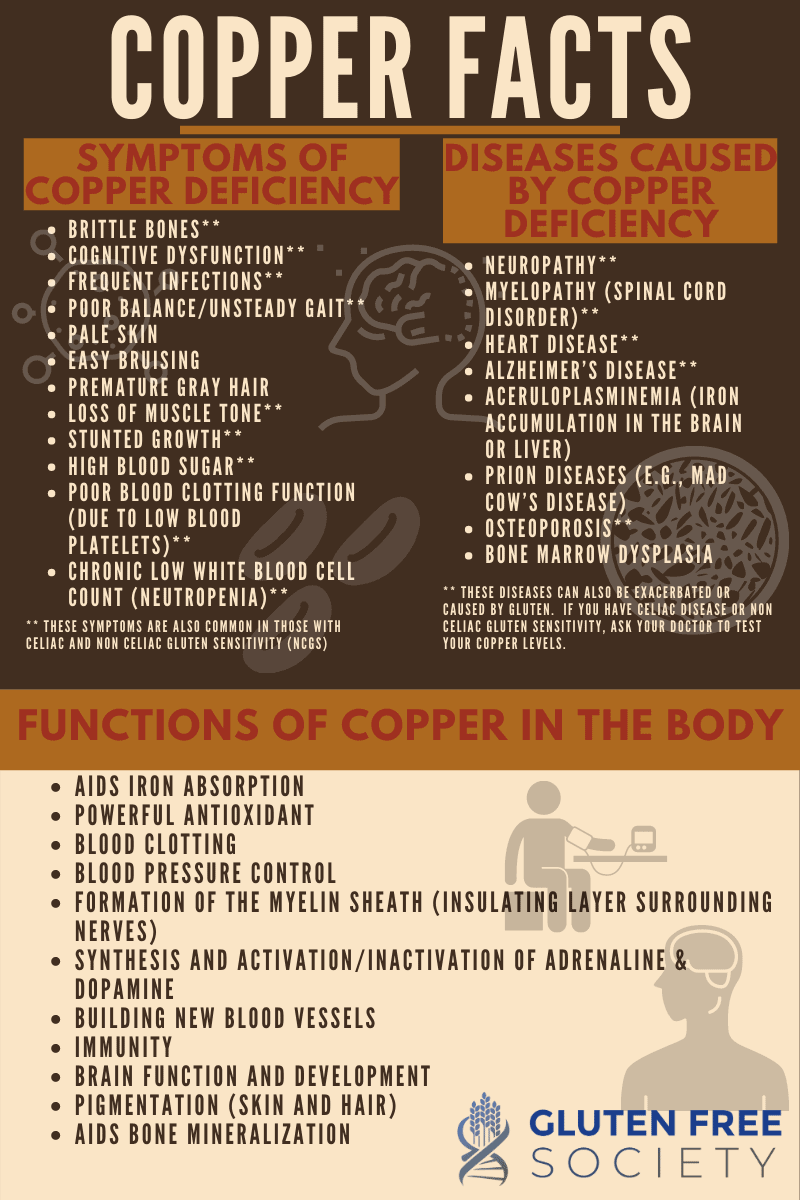

 Should Celiacs or Those with Gluten Sensitivity Be More Worried About Covid?
Should Celiacs or Those with Gluten Sensitivity Be More Worried About Covid?


 What Causes Leaky Gut – Going Beyond Gluten
What Causes Leaky Gut – Going Beyond Gluten