Can Gluten Cause Kidney Disease?
Your kidneys are located below your ribs and behind your stomach. And these two “bean-shaped” organs are involved in numerous vital functions, which include:
- Detoxification
- Blood pressure regulation
- Body fluid regulation
- pH regulation
- Vitamin D activation
- Red blood cell production
Inside your kidneys, you’ll find millions of small structures known as nephrons. Nephrons are responsible for filtering your blood to remove toxins and excess water, which gets eliminated through your urine.
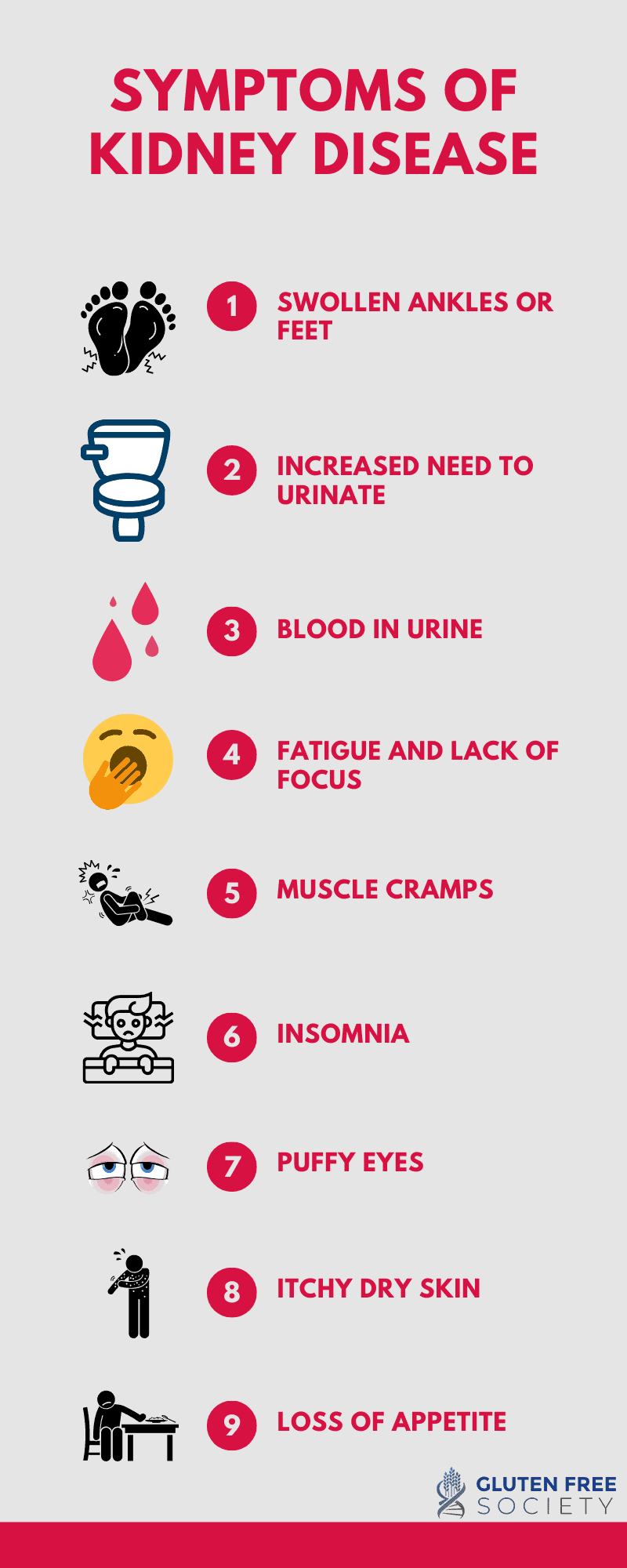
Many kidney diseases involve damage to the nephrons, which ultimately impairs detoxification. During the early stages of kidney disease, you may not experience symptoms. However, as the disease progresses, common symptoms include:
- Swollen ankles or feet
- Increased need to urinate
- Blood in urine
- Fatigue and lack of focus
- Muscle cramps
- Insomnia
- Puffy eyes
- Itchy, dry skin
- Loss of appetite
Can gluten cause kidney disease?
There’s evidence that gluten can contribute to the development of kidney disease. In fact, there are multiple case reports of individuals with kidney disease that are able to reduce or eliminate their medications as well as induce remission with a gluten-free diet.
Inflammation and Kidney Disease
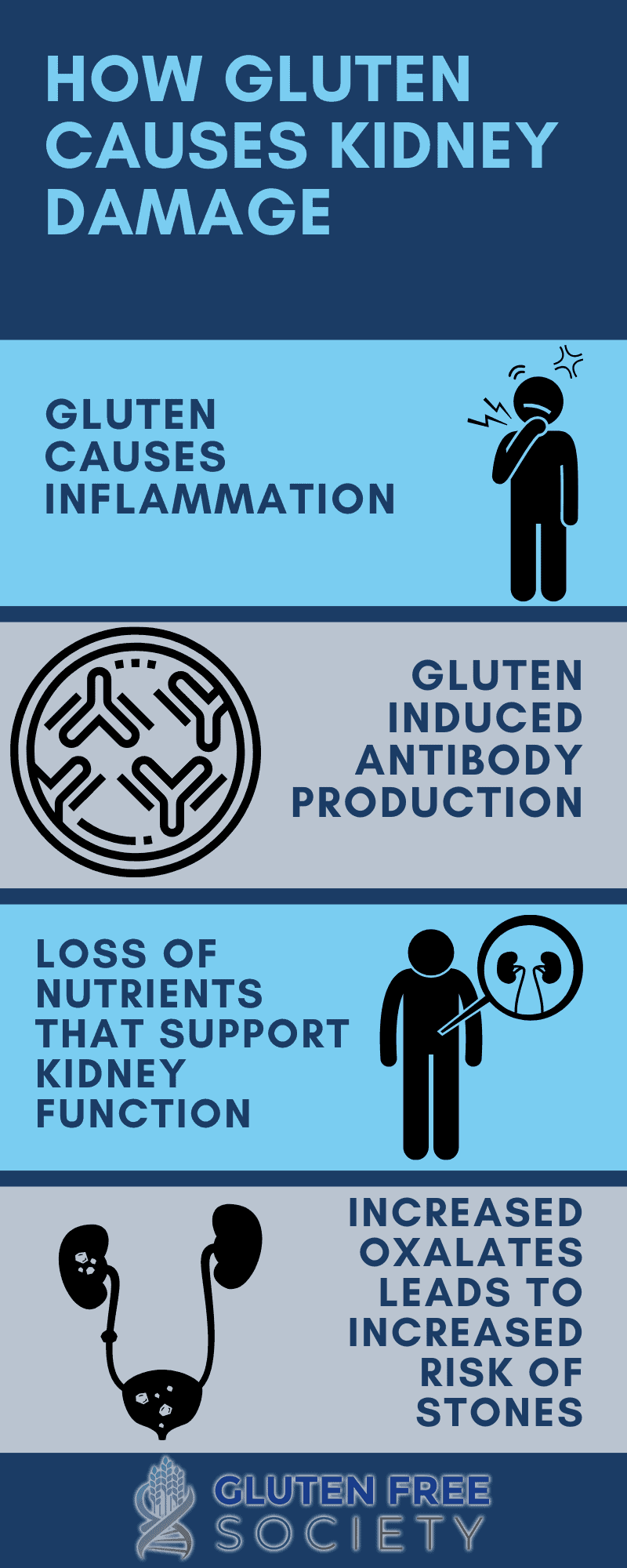
Gluten is a protein found in the seeds of grasses. And when consumed, it damages the lining of the gut in those with gluten sensitivity. This damage causes inflammation in the gut as well throughout the body.
When inflammation occurs in the kidneys, it can damage the kidney cells and lead to dysfunction and disease. In fact, gut inflammation has been detected in post-mortem studies of those with kidney disease.
Another gluten-related condition that often occurs and creates additional problems is called “leaky gut.” In a healthy gut, the cells lining the small intestine are tightly packed together. But when the gut is “leaky,” the tight junctions between the cells loosen, which then allows larger particles of undigested food, pathogens, and toxins to “leak” into the bloodstream.
This helps explain why studies have detected toxins released from gut bacterial (a.k.a. endotoxins) in the blood of those with kidney disease. And increased levels of endotoxins are associated with more severe inflammation as well as advanced stages of kidney failure.
Changes to the composition of gut bacteria are also often observed with both celiac disease and kidney disease. This can affect the immune system as well as lead to the build-up of pro-inflammatory toxins, which are also more likely to “leak” into the bloodstream.
Something else we can’t ignore is how systemic inflammation triggered by gluten can also increase one’s risk for other conditions, including high blood pressure, type 2 diabetes, and heart disease. And these conditions are considered risk factors for kidney failure.
Gluten and IgA Nephropathy
IgA nephropathy is also known as Berger’s disease. It involves the build-up of a substance known as IgA, which is a type of antibody. Antibodies are proteins produced by your immune system to attack foreign invaders.
Therefore, IgA is a good thing. But with Berger’s disease, IgA accumulates in the kidneys and causes inflammatory damage. As with other kidney diseases, over time it can affect the kidneys’ ability to filter waste from the blood.
Why IgA antibodies build up in the kidneys is not fully understood. Researchers suggest genetics and chronic infections are likely contributing factors. But gluten is also a suspected trigger.
Specifically, patients with Berger’s disease have been found to have high concentrations of IgA antibodies against gliadin, a gluten protein. Researchers have also been able to induce Berger’s disease in mice by feeding them gluten. And there are case reports of individuals healed with a gluten-free diet.
Common Nutrient Deficiencies
Because gluten causes intestinal inflammation and malabsorption, nutrient deficiencies are common among those with celiac and gluten sensitivity. Similarly, those with chronic kidney disease also have a higher risk of malnutrition due to decreased appetite, hormonal imbalances, metabolic dysfunction, and inflammation.
Zinc, selenium, folate, and vitamin B12 are just a few of the nutrient deficiencies that have been observed with both gluten-related conditions and kidney disease.
Zinc is a mineral found mostly in bone, but also in organs, including the kidneys. It plays hundreds of roles inside cells. For example, in the kidney, it’s involved in creating microtubules found inside renal nephrons responsible for filtering toxins from the blood.
Zinc and selenium play important roles in the body’s antioxidant defense system, which helps protect the kidneys from damage that could otherwise contribute to renal disease.
One study found that supplementing with 200 micrograms of selenium daily for 12 weeks significantly reduced inflammation and oxidative stress in those with kidney disease when compared to a placebo control group.
Folate is used by the kidneys to create a substance (erythropoietin) necessary to make red blood cells in the bone marrow. Thus, without an adequate supply of folate, anemia is a possibility.
In addition, studies have found that homocysteine levels in those with kidney disease are often high. Homocysteine is an amino acid made by your body and high levels are associated with inflammation. And folate and vitamin B12 are necessary to prevent the build-up of homocysteine in the blood.
Further, a study found that folate supplementation along with enalapril (a drug used to treat high blood pressure, diabetic kidney disease, and heart failure) significantly delayed the progression of kidney disease when compared to enalapril treatment alone.
Gluten and Processed Foods
The foods most people eat that contain gluten are heavily processed. Think bread, pasta, crackers, cookies, etc. And these foods promote a wide range of problems, including inflammation, obesity, type 2 diabetes, high blood pressure, and heart disease. All conditions linked to poor kidney health.
These connections exist because processed foods mostly contain quickly absorbed starch, sugar, and pro-inflammatory omega-6 fats. Plus, they lack fiber, protein, anti-inflammatory omega-3 fats, vitamins, and minerals.
Gluten and Kidney Stones
Kidney stones are hard deposits that form when urine becomes concentrated with minerals and other crystal-forming substances, such as uric acid and oxalates. And they’re painful as they pass through the urinary tract. Other symptoms include:
- Dark-colored urine
- Unusually smelling urine
- Nausea and vomiting
- Frequent urination
- Fever and chills
Uric acid is a natural by-product of foods that contain purines, such as seafood, alcohol, and some meats. Oxalates are natural compounds found in many foods.
Oxalates bind to calcium in your digestive tract and are eliminated through the stool. If they don’t bind to calcium, they travel in the blood to the kidneys and are excreted through urine.
A study found that those with untreated celiac disease have 120% more oxalates in their urine than healthy subjects. This may be the result of digestive-related issues associated with celiac disease. Diarrhea is also a common symptom associated with celiac disease that can cause dehydration and concentrated urine.
Thus, researchers suggest high concentrations of oxalates in the urine increase the risk of kidney stones in those with celiac disease. In the same study, researchers also found that treatment with a gluten-free diet reduced the concentration of oxalates in the participants’ urine as well as their risk of kidney stones.
Can Gluten Cause Kidney Disease? Sum It All Up
We can’t overlook the overwhelming evidence linking the effects gluten has on genetically susceptible individuals and kidney disease. Thus, it’s imperative to keep tabs on your kidney if you have celiac disease or gluten sensitivity. Similarly, if you’re diagnosed with kidney disease, talk with your doctor about eliminating gluten from your diet. It might be an important and critical step in your recovery.
The post Can Gluten Cause Kidney Disease? appeared first on Gluten-Free Society.
No comments:
Post a Comment